Neurology can be hard, but I made it super easy for you! Just read this blog 2 or 3 times, and you’ll understand it. I made everything as simple as possible you’re going to love it!
1. Huntington’s Disease (HD)
1. What is it?
A brain disorder that causes strange body movements, like dancing movements.
2. How it spreads?
It is a autosomal dominant and runs in families. The problem is on chromosome number 4 with too many CAG repeats in a gene.
3. What is anticipation?
The disease starts earlier and is worse in the next generation. like more it pass will become severe to next generation.
4. What are the Symptoms?
- Memory loss (dementia)
- Slow, jerky movements (chorea)
- Confused thinking (AlOC)
- Sudden falls or fainting
5. What are the tests?
Only 2 tests are done that are following.
- Genetic test is the gold standard to confirm
- CT or MRI shows brain shrinking (cerebral atrophy)
6. What is the treatment?
No cure yet. Only supportive care.
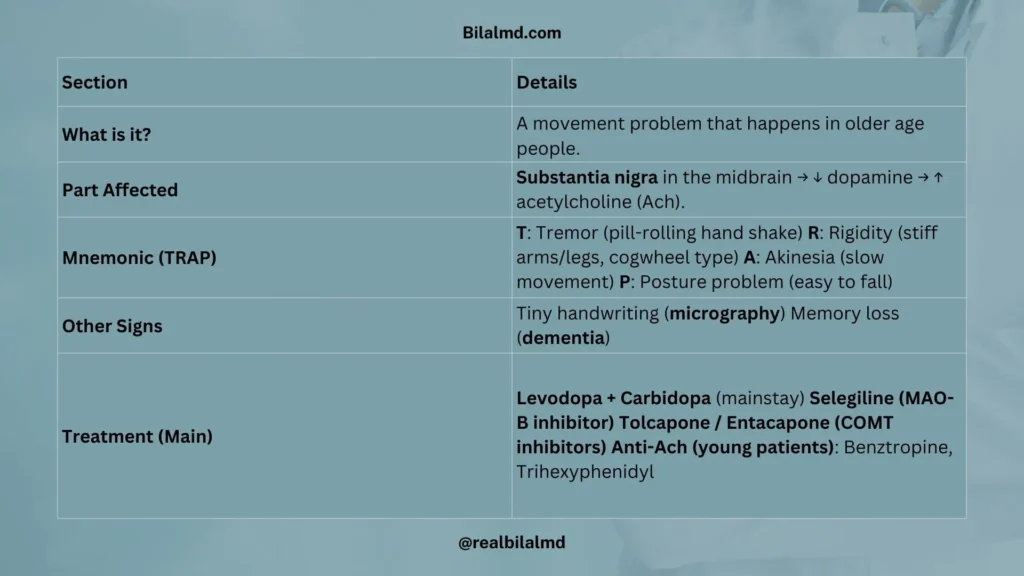
2. Parkinson’s Disease
1. What is it?
A movement problem that happens in older age people.
2. Which part is affected?
Substantia nigra is affected which lies in the midbrain, where dopamine decreases that increases acetylcholine (Ach).
3. How to remember?
We use “TRAP” mnemonic to remember Parkinson’s Disease.
- T: Tremor (hand shaking like rolling a pill)
- R: Rigidity (stiff arms/legs, like a cogwheel)
- A: Akinesia (moves slowly)
- P: Posture problem (easy to fall)
4. Other signs
- Tiny handwriting (micrography)
- Memory loss (dementia)
5. Treatment
- Levodopa + Carbidopa
Mao monoamine oxidase (MAO) andcatechol-o-methyl transferase (COMT) are dopamine antagonist.
2. Selegiline is MAO type B inhibitor means it keeps dopamine to work for long time.
3. Tolcapone and Entacapone = (Ropinirole, Bromocriptine)
- These are COMT inhibitors.
- They help dopamine last longer in the brain.
- Used with other Parkinson’s medicines (like Levodopa).
- They don’t work alone — they are part of combination therapy.
4. For young people Anti-Ach drugs Benztropine, Trihexyphenidyl are given but they have side effects like
- Dry mouth,
- Constipation
- Urine retention
- Dry eyes.
How Levodopa and Carbidopa Work
- Levodopa is the main medicine. It helps make dopamine in the brain.
- If we give Levodopa alone, a body enzyme called dopa decarboxylase enzyme (outside the brain) changes it too early. Carbidopa is added to protect Levodopa in the body.
- Carbidopa stops Levodopa from working before it reaches the brain.
- Carbidopa cannot enter the brain (it stops at the brain barrier).
- Levodopa goes into the brain and then works to fix low dopamine.
Think of it like this:
Carbidopa is a bodyguard that keeps Levodopa safe until it reaches the brain.
Once inside, Levodopa does its job.
3. Neuromuscular Junction Disorders
There are two types of NMJ disorders
- Myasthenia gravis
- Lambert-Eaton Syndrome
1. Myasthenia Gravis
In Myasthenia Gravis, the body makes anti-Ach receptor antibodies that block the Ach (acetylcholine) receptors at the muscles.
This stops the message from the nerve to the muscle, so the muscles become weak.
- In the morning, the person feels okay.
- By evening, they feel very tired.
- Working or moving makes the weakness worse.
- Ocular symptoms are present.
Eye symptoms (ocular signs)
- Ptosis – Drooping eyelids
- Diplopia – Double vision

Linked with
- Thymoma – A tumor in the thymus glands
2. Lambert-Eaton Syndrome
Calcium is needed to release Ach from Axon. In Lambert eaton syndrome anti-calcium channel antibodies are formed and it act on the calcium channel and wont allow to release Ach. Simply no calcium no ach. In morning they are very tired but with movement they become better. There is no ocular symptoms.
Linked with
- Small Cell Lung Cancer
Small cell lung cancer arise from center of lungs and it produce
- Ectopic ACTH → Causes Cushing’s signs
- Ectopic ADH → Causes SIADH (low sodium)

Diagnosis
- Myasthenia gravis is diagnosed by edrophonium (Tensilon) test and anti-Ach receptor antibodies.
- Lambert eaton syndrome is diagnosed by edrophonium test.
- Edrophonium temporary decreases Ach esterase (ach breaker) and will increase Ach.
Treatment
Pyridostigmine – keeps more Ach in the junction to improve strength.
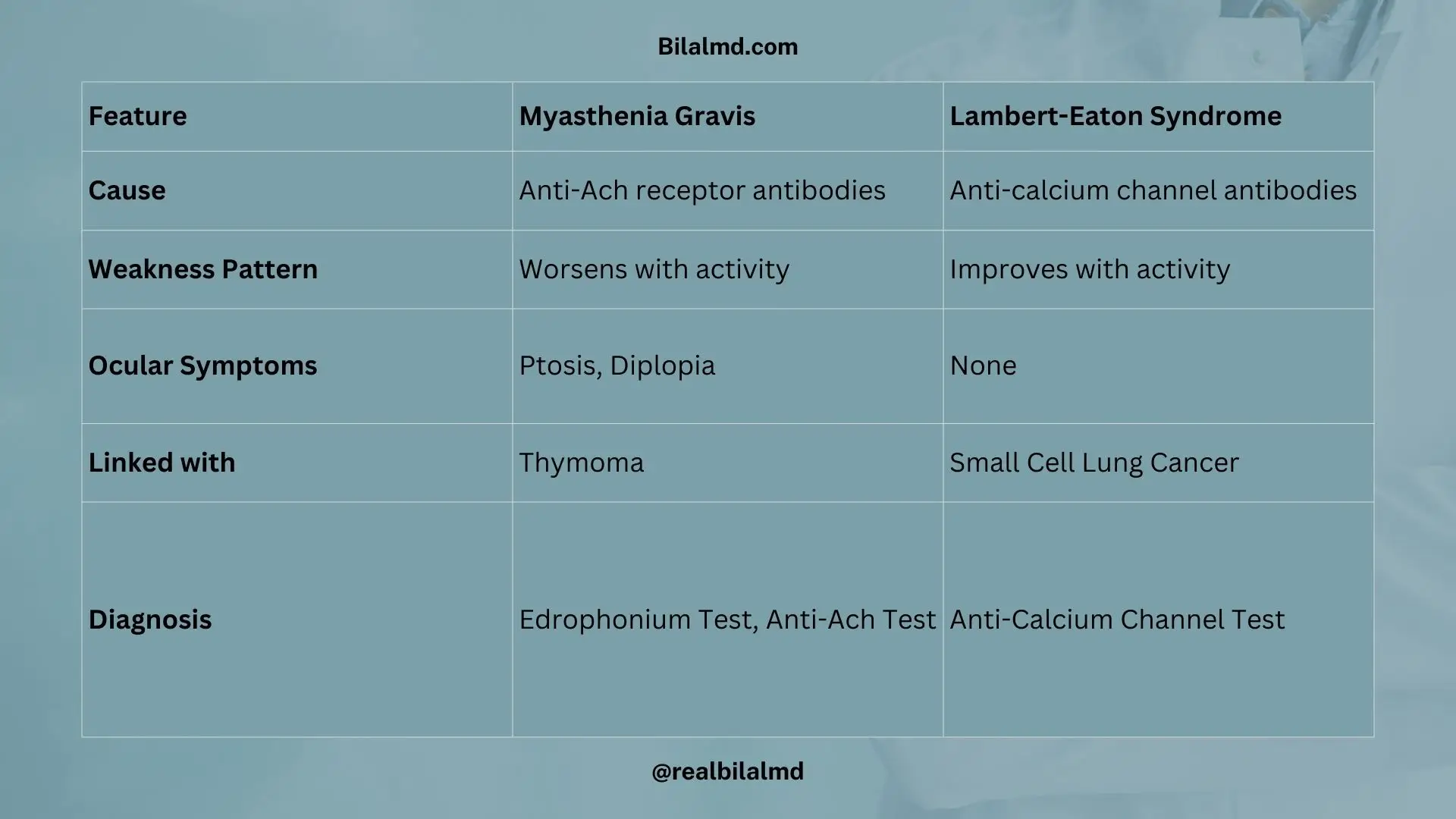
| Feature | Myasthenia Gravis | Lambert-Eaton Syndrome |
| Cause | Anti-Ach receptor antibodies | Anti-calcium channel antibodies |
| Weakness Pattern | Worsens with activity | Improves with activity |
| Ocular Symptoms | Ptosis, Diplopia | None |
| Linked with | Thymoma | Small Cell Lung Cancer |
| Diagnosis | Edrophonium Test, Anti-Ach Test | Anti-Calcium Channel Test |
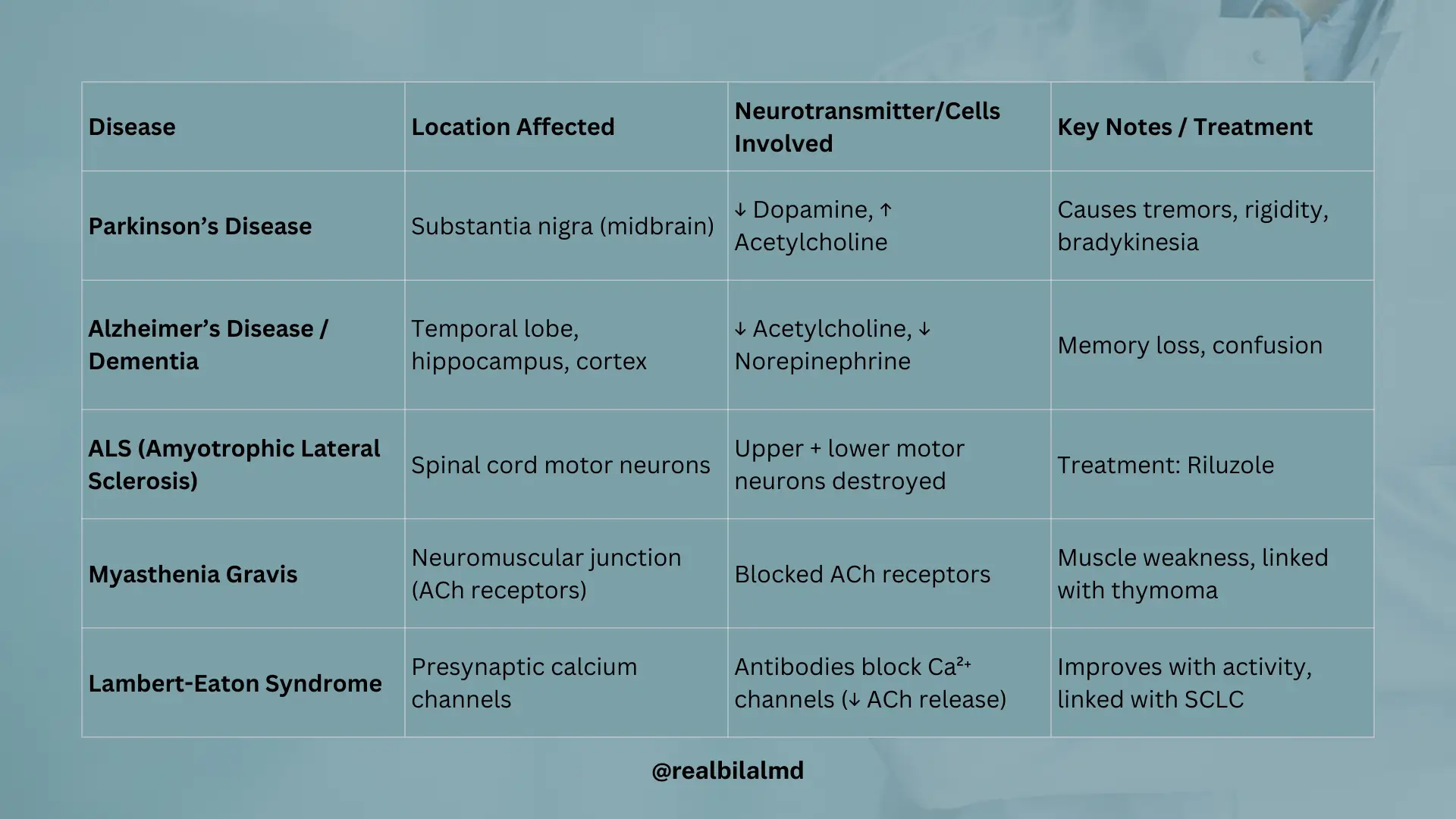
3. Location of Cell Death According To Disease
- Parkinson’s Disease: Substantia nigra is damaged. Dopamine goes down and acetylcholine (Ach) goes up.
- Alzheimer’s + dementia Disease: Effects the temporal lobe. Ach and norepinephrine go down.
- ALS (Amyotrophic Lateral Sclerosis): Destroys spinal cells. Both upper and lower motor nerves are affected. Treatment: Riluzole
- Myasthenia Gravis: The body blocks Ach receptors → muscles become weak.
- Lambert-Eaton Syndrome: The body makes antibodies against calcium channels (Anti-cac).
4. Tremors (Shaking)
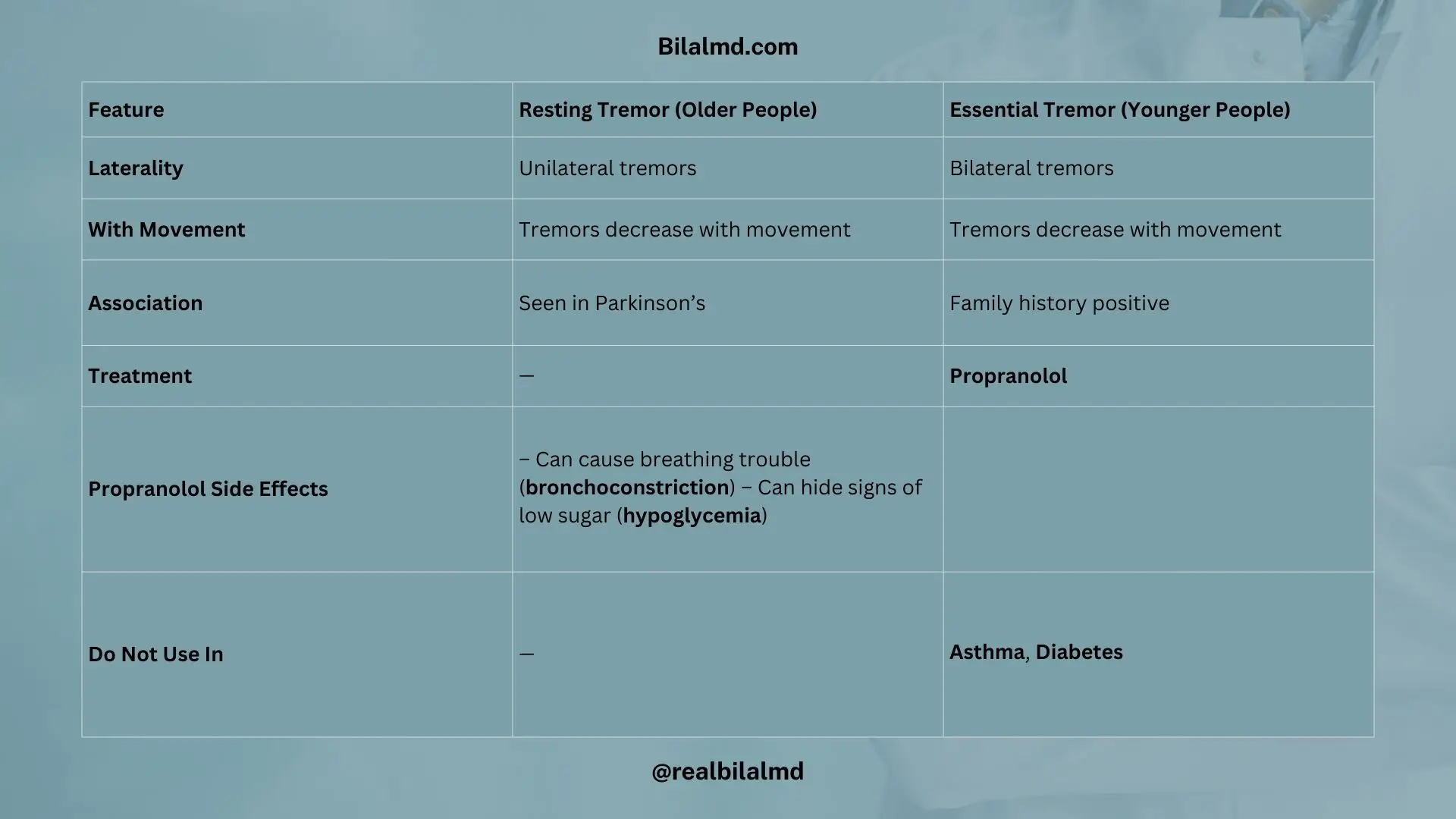
| Older People – Resting Tremor | Younger People – Essential Tremor |
| Unilateral tremors | Bilateral tremors |
| Tremors decrease with movement | Tremors decrease with movement |
| Seen in Parkinson’s. | Family history positive |
| Treatment: Propranolol Side Effects: 1. Can cause breathing trouble (bronchoconstriction) 2. Can hide signs of low sugar (hypoglycemia) Do Not Use In: 1. Asthma 2. Diabetes |
Tremor:
Can be caused by Graves’ disease (hyperthyroidism).
5. Intracerebral Hemorrhage (ICH)
The brain is covered by 3 protective layers called meninges:
- Dura mater – outer layer (strongest)
- Arachnoid mater – middle layer
- Pia mater – inner layer (touches the brain)
Spaces between layers:
- Epidural space – above the dura mater and skull
- Subdural space – below the dura mater and arachnoid mater
- Sub-arachnoid space – below the arachnoid mater and brain
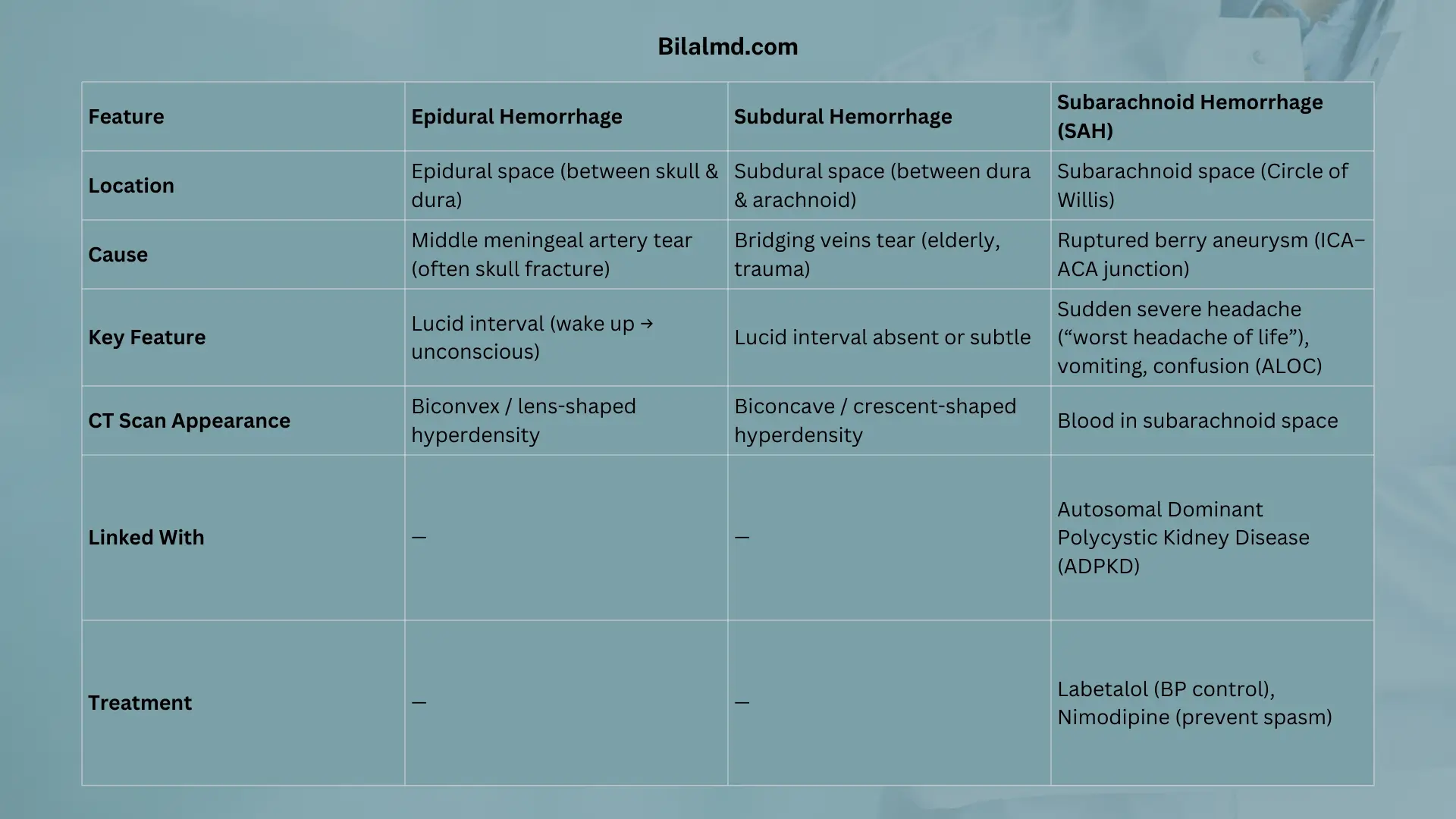
Types of Brain Bleeding (Hemorrhage)
There are three types of bleeding occur in brain
- Epidural Hemorrhage
- Subdural Hemorrhage
- Subarachnoid Hemorrhage
1. Epidural Hemorrhage
- Blood collects in the epidural space
- Cause: Middle meningeal artery tear (often from skull fracture)
- Lucid interval: Person wakes up then goes unconscious
- CT scan: Looks like a biconvex (lens-shaped) bleed
2. Subdural Hemorrhage
- Blood collects in the subdural space
- Cause: Bridging veins tear (common in elderly or after trauma)
- Lucid interval: May or may not happen
- CT scan: Looks like a biconcave (crescent) bleed

| Feature | Epidural Hemorrhage | Subdural Hemorrhage |
|---|---|---|
| Location | Epidural space (between skull and dura) | Subdural space (between dura and arachnoid) |
| Primary Cause | Tear of middle meningeal artery (often from skull fracture) | Tear of bridging veins (common in elderly or after trauma) |
| Lucid Interval | Classic “wake-up” then rapid decline | May be absent or subtle, variable timing |
| CT Scan Appearance | Biconvex (lens-shaped) hyperdensity | Biconcave (crescent-shaped) hyperdensity |
3. Sub-arachnoid Hemorrhage (SAH)
- Bleeding collects in the subarachnoid space (Circle of Willis)
- Cause: Rupture of berry aneurysm (small weak spot in artery)
- Most common at: Where Internal Carotid meets Anterior Communicating Artery
Symptoms:
- Sudden severe headache (“worst headache of life”)
- Vomiting, nausea, confusion (ALOC = altered level of consciousness)
Linked to:
- Autosomal Dominant
- Polycystic Kidney Disease
Treatment:
- Beta blockers (Labetalol) – to control blood pressure
- Calcium channel blockers (Nimodipine) – to prevent vessel spasm
Extra Notes:
- Vertebral artery passes through the foramen magnum (big hole at the base of the skull).
- Internal carotid artery passes through the foramen lacerum (a smaller hole near the base of the skull).
6. Multiple Sclerosis (MS)
An immune-mediated disease that attacks the central nervous system (CNS) and damages the myelin sheath (the protective covering of nerves).
Key Features
- Age group: 20–40 years
- Gender: 3(females) : 2(males)
- Worsens with hot showers
- Improves during pregnancy
- Relapsing-remitting pattern (symptoms come and go)

Symptoms
Remember the mnemonic “SIN“
- S – Scanning speech (broken, choppy speech)
- I – Intention tremor (tremor increases during movement)
- N – Nystagmus (eye shaking) → can cause diplopia (double vision)
Diagnosis
- Investigation of choice: MRI (shows white matter plaques)
- Diagnostic criteria: McDonald’s Criteria
Treatment
- First-line: Oral corticosteroids
- If no response: Plasma exchange (plasmapheresis)
- If optic neuritis (eye involvement):
Start with IV steroids, then oral steroids, then plasmapheresis
New Therapy
- Ocrelizumab – a monoclonal antibody used in MS treatment

Here are other materials for NLE NRE step 1
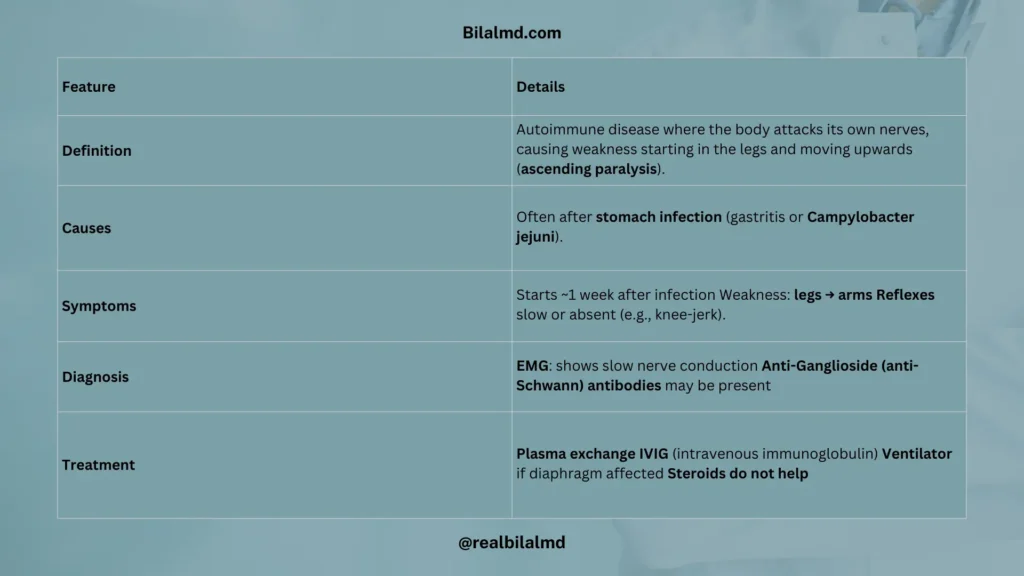
7. Guillain-Barré Syndrome (GBS) / Acute Inflammatory Polyneuropathy
A sickness where the body attacks its own nerves (auto immune). It causes weakness that starts in the legs and moves up (ascending paralysis).
Causes
- Often happens after a stomach infection (gastritis or campylobacter jejuni)
Symptoms
- Starts about 1 week after the infection
- Legs feel weak, then arms
- Reflexes (like knee-jerk) are slow or gone
Diagnosis
- EMG: Shows slow nerve conduction
- Anti-Ganglioside (anti-Schwann) antibodies may be present
Treatment
- Plasma exchange
- IVIG (good antibodies through a drip)
- Ventilator if the diaphragm is affected
- Steroids don’t help
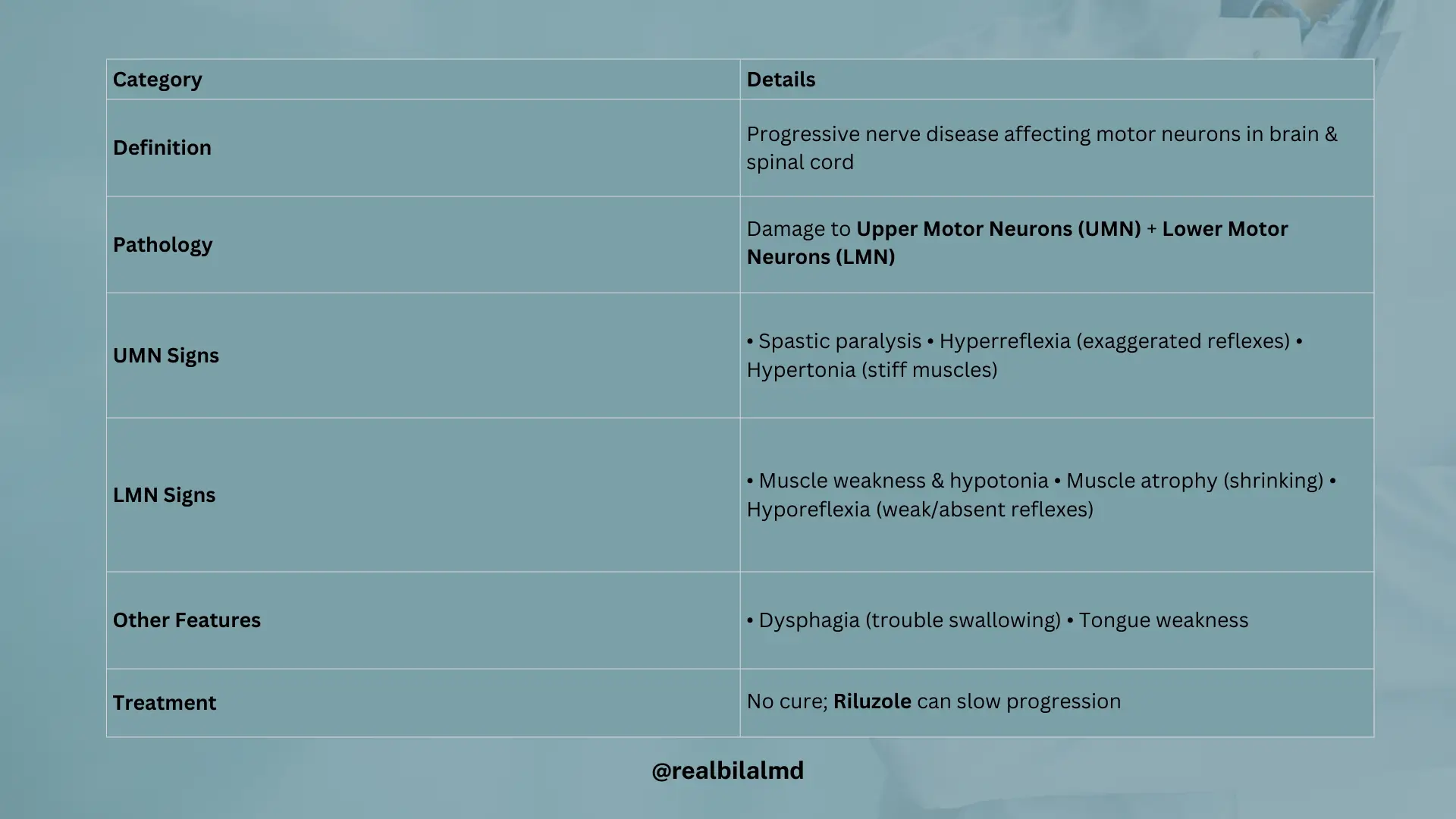
8. Amyotrophic Lateral Sclerosis (ALS) / Lou Gehrig’s Disease
What is ALS?
ALS is a sickness that affects the nerves that help your muscles move. These nerves come from the brain and spine.
What happens in ALS?
Two types of nerves stop working:
- Upper motor nerves – from the brain (UMN)
- Lower motor nerves – from the spine (LMN)
Signs of Upper Motor Nerve Damage:
- Muscles become stiff (Spastic paralysis)
- Reflexes are too strong (Hyperreflexia)
- Hard to move arms or legs (Hypertonia)
Signs of Lower Motor Nerve Damage:
- Muscles become soft and weak (hypotonia)
- Muscles shrink (muscle atrophy)
- Reflexes are very slow or gone (hyporeflexia)

Other Problems:
- Trouble swallowing food
- Hard to move the tongue
Treatment:
There is no full cure, but a medicine called Riluzole helps slow it down.
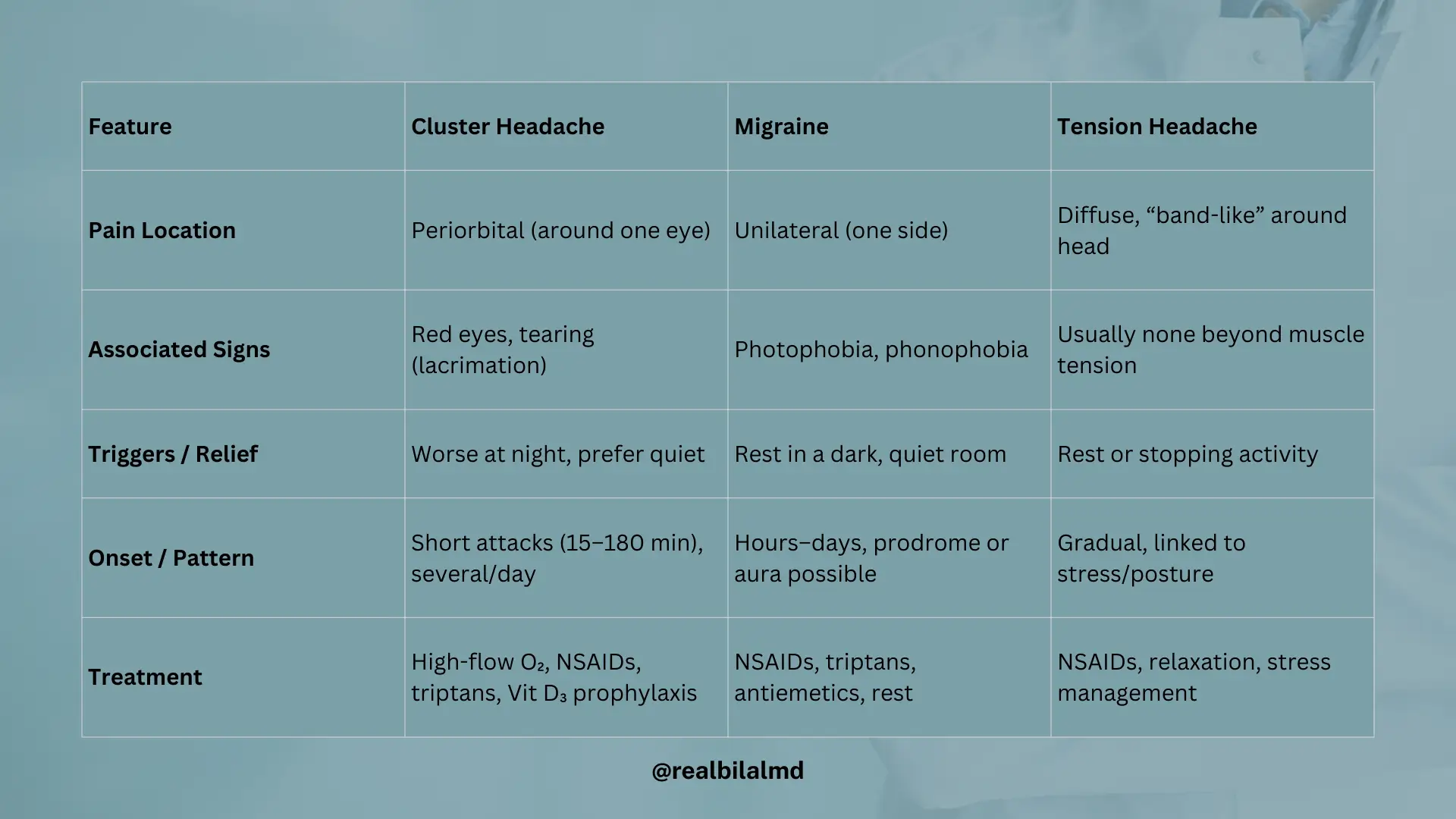
9. Headache
Headache Types
There are 2 main types of headache:
- Primary Headache – No cause (it happens by itself)
- Secondary Headache – Has a cause (like fever, injury, infection)
Types of Primary Headaches
1. Cluster Headache
- Pain around the eye (periorbital)
- Red eyes, tears and lacrimation
- Releive in dark places
- Treatment: NSAIDs, Vitamin D3
2. Migraine
- One side of head hurts (unilateral)
- More common in females
- Pain worse with light and noise
- Treatment: NSAIDs, rest in dark room
3. Tension Headache
- Pain gets worse with work/activity
- Relieves with rest
- Treatment: NSAIDs

| Feature | Cluster Headache | Migraine | Tension Headache |
|---|---|---|---|
| Pain Location | Periorbital (around one eye) | Unilateral (one side of head) | Diffuse, tight “band-like” around head |
| Associated Signs | Red eyes, tearing (lacrimation) | Photophobia, phonophobia (light/sound worsens pain) | None typically beyond aching muscle tension |
| Triggers/Relief | Prefer dark, quiet environment | Rest in a dark room | Rest or cessation of activity |
| Onset/Pattern | Short attacks (15–180 min), several per day, often at night | Hours to days, may have prodrome or aura | Gradual onset, related to stress or posture |
| Treatment | High-flow oxygen, NSAIDs, triptans; sometimes prophylactic Vitamin D₃ | NSAIDs, triptans, antiemetics, rest in dark room | NSAIDs, relaxation techniques, stress management |
10. Seizure
A seizure happens when brain cells (neurons) become too active (excite)that lead to muscle contraction. This can make the body shake or jerk.
Why do seizures happen?
- Seizures due to low or high salts (electrolyte imbalance) in the body leads to acquired seizures.
- Seizures due to defect in genes or environmental issues leads to idiopathic seizures.
What is Epilepsy?
When someone has seizures again and again, it’s called epilepsy.
Types of Seizure
- Partial Seizure (only a part of the brain):
- Simple Seizure: The person is awake with seizure.
- Complex Seizure: The person is confused or not awake with seizure. Often starts in the temple part of the brain.
- Generalized Seizure (whole brain):
- Affects both sides of the brain.
- Person passes out (ALOC) with seizure.
- Tonic-clonic seizure:
- ALOC, back extend and muscle constrict.
- Bite tongue and pee without knowing (urine incontinence).
- Absence Seizure (common in children):
- Child stares or blanks out for 5–10 seconds.
- No shaking.
- Status Epilepticus (vey long seizure)
Lasts more than 5 minutes – very dangerous.- Give benzodiazepines and fosphenytoin.
- May need to ventilate
Diagnosis
We do a test called EEG to look at brain activity.
Treatment
- Secure the airway so they can breathe.
- Medicines called antiepileptics help stop seizures.
Medicine Tips
- Valproic acid is the liver toxic.
- Phenytoin blocks sodium channel (Na) – helps stop seizures also it is a anti arrhythmic drug.
- Phenytoin side effects:
- Swollen gums (Gingival hyperplasia).
- Megaloblatic Anemia.
- Also works as a antiarrythemic.
- Antiepileptics (hepatotoxic) medicines can cause low folate:
- Can lead to spina bifida (a birth problem).
- Can cause megaloblatic anemia (low blood).
- Best drug for absence seizure: Ethosuximide
11. Dementia
- Dementia means losing memory and thinking skills slowly, mostly in older people.
- The brain gets smaller over time.

Types of Dementia
1. Alzheimer’s Disease
- Most common kind.
- Brain gets smaller and ventricles (fluid spaces) get bigger.
- Senile Plaques (bad proteins) build up in the brain.
- Symptoms: Forgetting things, trouble thinking, confusion.
- Medicines: Donepezil, Galantamine.
2. Normal Pressure Hydrocephalus (NPH)
- Brain’s fluid spaces (ventricles) get bigger (ventriculomegaly), but fluid pressure stays normal.
- Brain may shrink.
- Main signs:
- Ataxia (Walking problems)
- Dementia
- Urinary incontinence
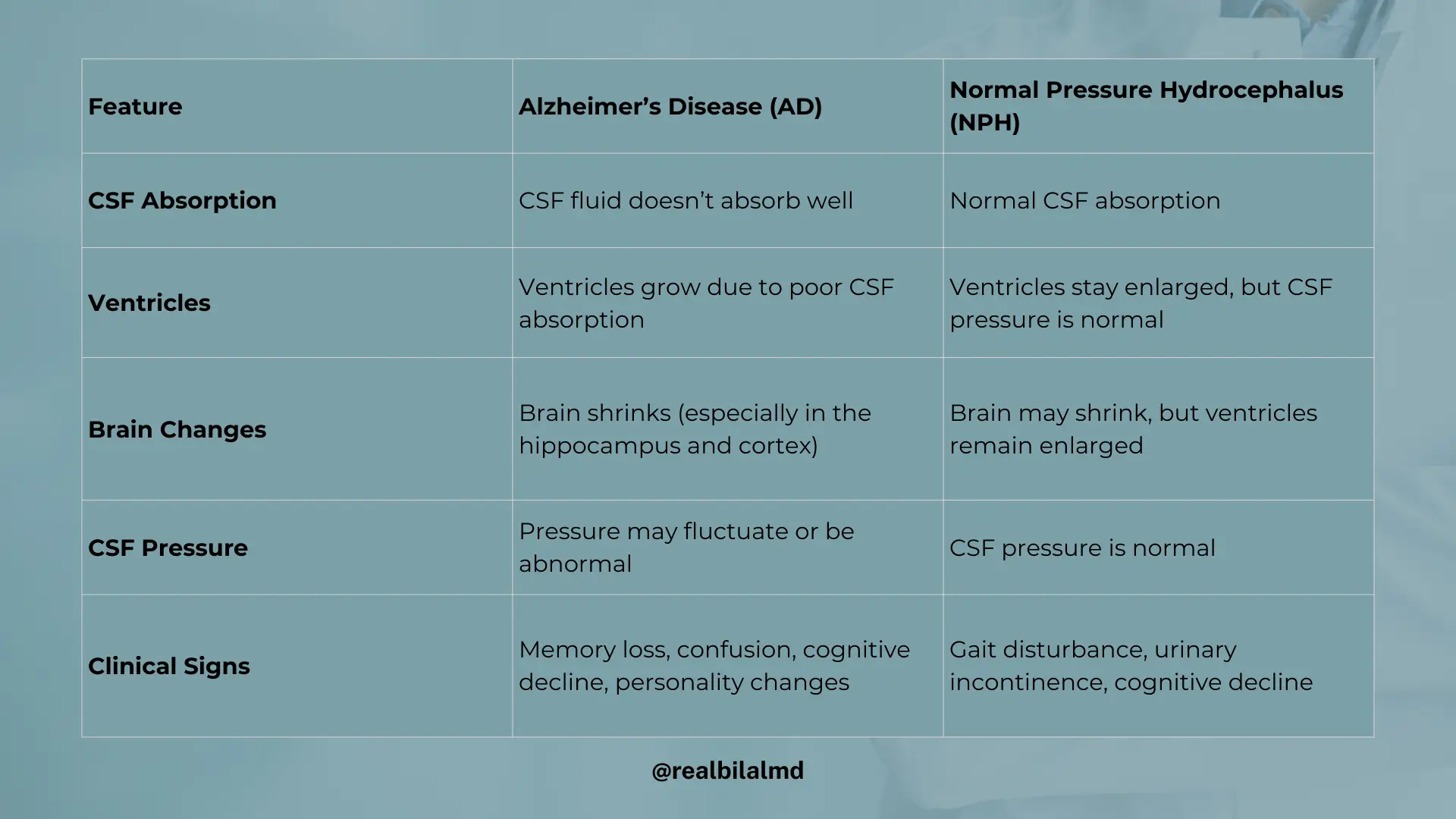
| Feature | Alzheimer’s Disease (AD) | Normal Pressure Hydrocephalus (NPH) |
|---|---|---|
| CSF Absorption | CSF fluid doesn’t absorb well | Normal CSF absorption |
| Ventricles | Ventricles grow due to poor CSF absorption | Ventricles stay enlarged, but CSF pressure is normal |
| Brain Changes | Brain shrinks (especially in the hippocampus and cortex) | Brain may shrink, but ventricles remain enlarged |
| CSF Pressure | Pressure may fluctuate or be abnormal | CSF pressure is normal |
| Clinical Signs | Memory loss, confusion, cognitive decline, and personality changes | Gait disturbance, urinary incontinence, and cognitive decline |
3. Lewy Body Dementia
- Dementia with hallucinations (seeing or hearing things that aren’t real).
4. Frontotemporal Dementia (Pick’s Disease)
- Front and temporal parts of the brain decrease in size.
- Causes behavior changes like acting oddly or saying strange things.
- Dementia
5. Memory Loss (Amnesia)
- Happens suddenly, often after a head injury or stress.
Types of Amnesia:
- Retrograde Amnesia:
- Can’t remember things before the accident.
- Anterograde Amnesia:
- Can’t remember things after the accident.
6. Vascular Dementia
- Second most common type of dementia.
- Happens after many strokes with dementia and multiple infarction.
7. Creutzfeldt-Jakob Disease (CJD)
- Demenntia that comes very suddenly.
- Caused by prion proteins (bad proteins) in the brain.
12. Stroke
- A stroke happens when blood can’t reach the brain.
- Middle cerebral artery is affected that is the branch of internal carotid artery.
- This causes brain damage and problems like moving, talking, or seeing.
Types of Stroke:
- Ischemic Stroke (80–85%): A block in the blood vessel.
- Hemorrhagic Stroke (10–15%): A burst in the blood vessel causing bleeding.
Stroke Risk Factors
Things that make stroke more likely remember by this mnemonic ‘LPDS’
- L: Hyper lipidemia (High cholesterol)
- P: Pressure of blood increases
- D: Diabetes
- S: Smoking
Arteries Affected in Stroke & Symptoms
- MCA (Middle Cerebral Artery) block
- Half body weakness, trouble speaking, face droops.
- Use ‘F.A.S.T’ mnemonic:
- Face: Is it drooping?
- Arm: Can they lift both arms?
- Speech: Is speech slurred?
- Time: Call an ambulance fast!
- PCA (Posterior Cerebral Artery) block
- Stroke with vision problems.
- ACA (Anterior Cerebral Artery) block
- Stroke with leg or lower body weakness.
Stroke Treatment
- If patient comes within 4 hours:
- Give TPA (Thrombolytics – a medicine to break the clot).
- If later than 4 hours:
- Give Aspirin (stops more clots by blocking TXA2).
13. Aphasia – Trouble Speaking or Understanding
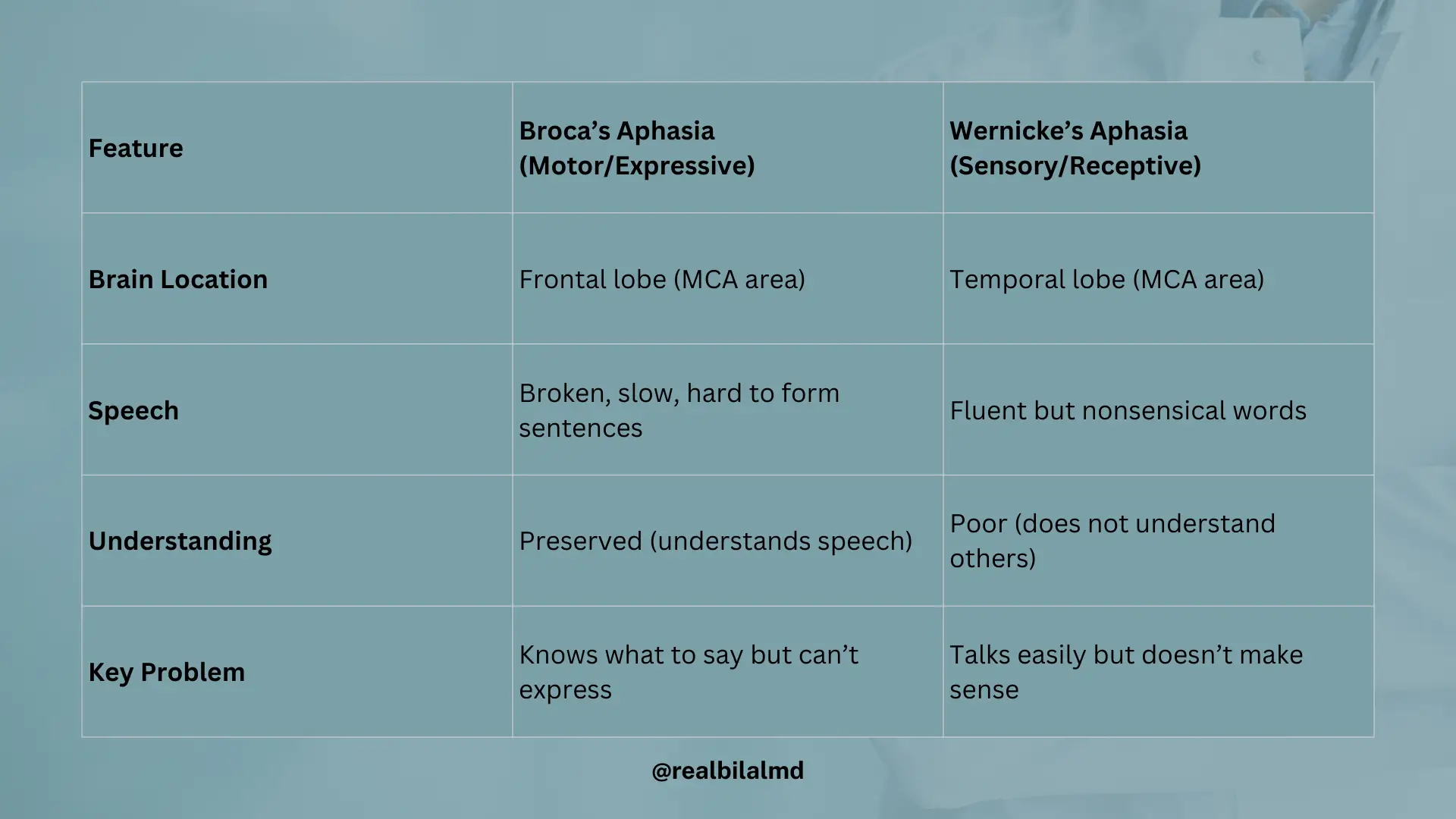
1. Broca’s Aphasia (Motor/Expressive Aphasia)
- Where in brain: Front part (frontal lobe), MCA area.
- What happens:
- Person understands what you say.
- But they can’t speak clearly or make full sentences.
- They know what they want to say but can’t get the words out.
2. Wernicke’s Aphasia (Sensory/Receptive Aphasia)
- Where in brain: Side part (temporal lobe), MCA area.
- What happens:
- Person can talk, but the words don’t make sense.
- They don’t understand what others are saying.
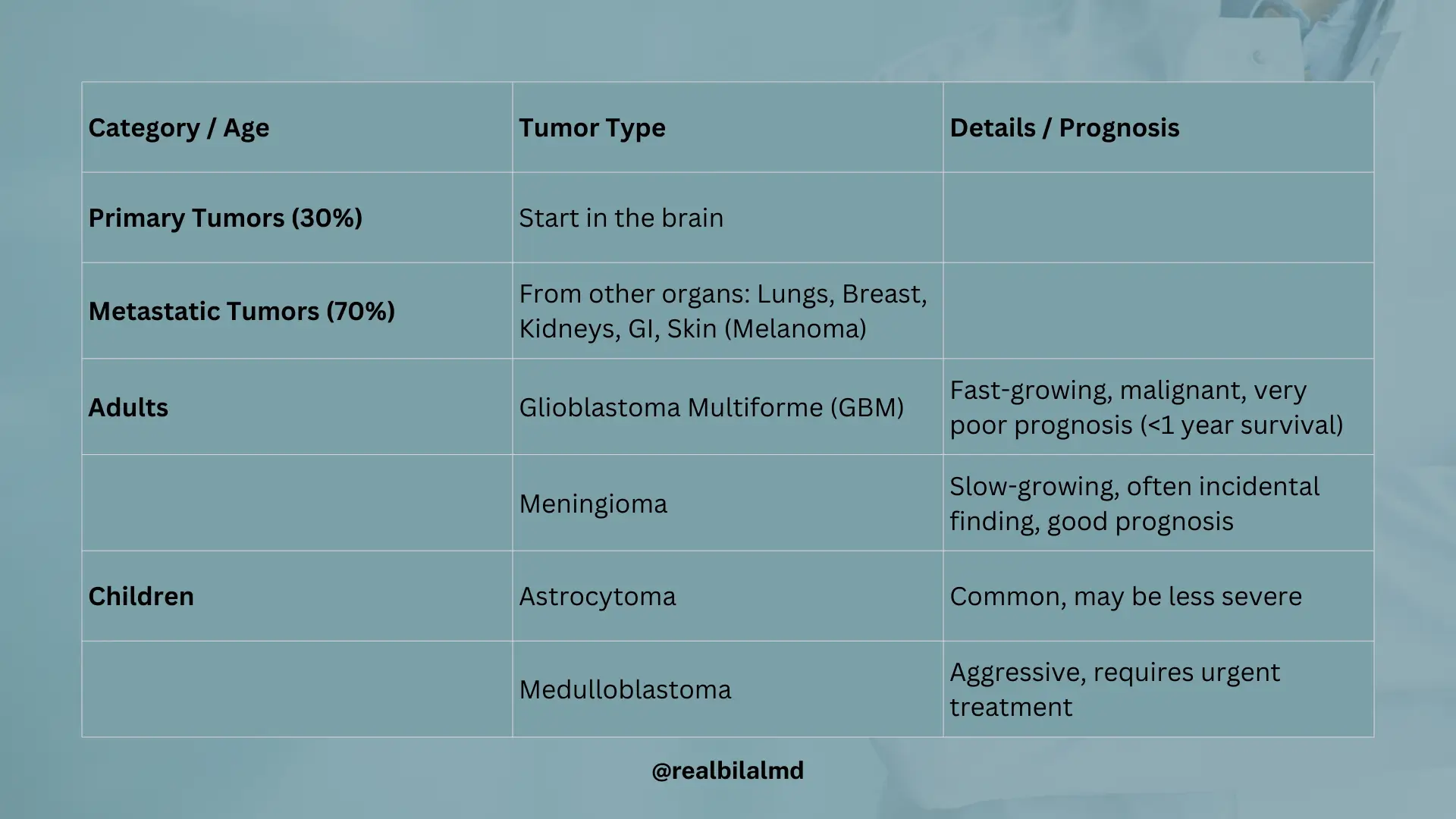
14. Brain Tumors (Neoplasms)
Types of Brain Tumors
- Primary Tumors (30%)
- These start in the brain.
- Metastatic Tumors (70%)
- These come from other parts of the body like:
- Lungs
- Breast
- Kidneys
- Stomach/Intestines (GI)
- Skin (Melanoma)
- These come from other parts of the body like:

Primary Brain Tumors by Age
In Adults:
- Glioblastoma Multiforme (GBM)
- Very fast-growing and dangerous.
- Malignant.
- Bad outlook (poor prognosis).
- Life less than 1 year.
- Meningioma
- Grows slowly.
- Headache and accidently diagnose.
- Usually not dangerous (good prognosis).
In Children:
- Astrocytoma
- Common and may be less severe.
- Medulloblastoma
- More aggressive.
- Needs fast treatment.
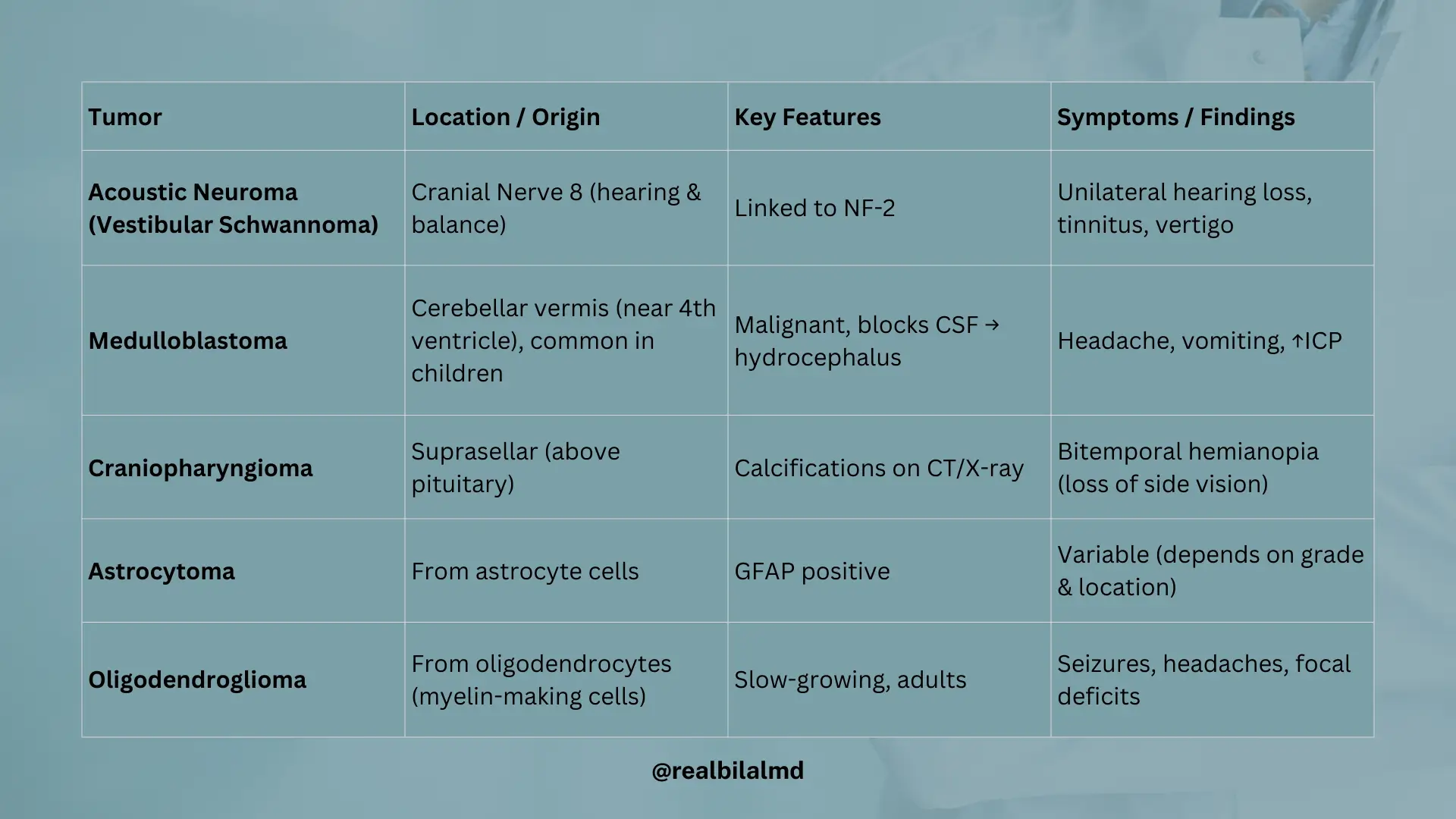
1. Acoustic Neuroma (Cranial Nerve 8 Tumor)
- Also called Vestibular Schwannoma.
- Seen in Neurofibromatosis Type 2.
- Affects Cranial Nerve 8, which helps with hearing and balance.
Symptoms:
- Hearing loss on one side.
- Ringing in the ears (tinnitus).
- Feeling dizzy or off balance (vertigo).
2. Medulloblastoma
- Common in children.
- Grows near the 4th ventricle in a part of the brain called the cerebellar vermis.
Symptoms:
- Blocks fluid in the brain → causes hydrocephalus (CSF buildup).
- Increased pressure in the head – intracranial pressure (ICP) (causing headache, vomiting).
3. Craniopharyngioma
- A tumor found above the pituitary gland (suprasellar area) Supra cellular tumor.
- Often shows calcium spots on X-rays or CT.
Symptoms:
- Calcium deposit on the optic chiasm (vision nerve crossing).
- Causes bitemporal hemianopia (can’t see side vision on both eyes).
4. Astrocytoma
- A brain tumor made from astrocyte cells.
- Test marker: GFAP (Glial Fibrillary Acidic Protein).
5. Oligodendroglioma
- A tumor made from oligodendrocytes (oligodendrocytes makes myelin shealth).
- Usually slow-growing and found in adults.